” John is an experienced Chief Executive Officer with a demonstrated history of working on a collaborative basis with like-minded organizations to accomplish mutually aligned goals.”

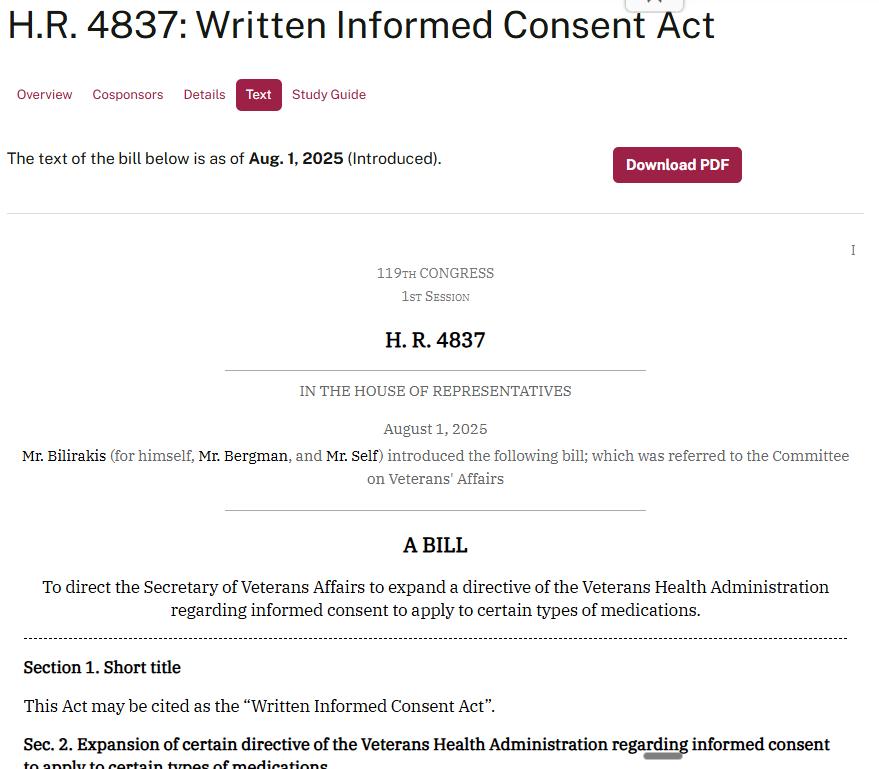
Congressman Gus Bilirakis introduces the Written Informed Consent Act! HR 4837
Here is a a show I did on the Lynne Haggerman Podcast.
Combatting Veteran Suicide
John Spagnola, President & CEO of Veterans Strategic Solutions, works to combat veteran suicide by focusing on the impact of trauma. He emphasizes the dangers of using anti-psychotic stimulants and benzodiazepines, which he believes can contribute to the mental health crises faced by veterans.
MG Jeff Phillips, former Executive Director of Reserve Officers Association, speaks on Written Informed Consent.
AUSN Discusses the Need for Informed Written Consent for Veteran Health
LCDR Steven Rogers, Operations Manager of the Association of the U.S. Navy, interviews veteran advocates Sherman Gillums, Jr., Ed.D. (USMC, Ret.) and John Spagnola about how to reduce the risk of suicide among military veterans by improving their access to written informed consent about risks of psychotropic medications and alternative treatments that are available.
Veteran Service Organizations and social and medical organizations are among some of the organizations John has been successful in establishing meaningful relationships.
John has also formed relationships with Congress and Committee members with the intention of bettering the lives of veterans and their families.
As a result of the above relationships, John has been instrumental in linking a Congressional Sponsor and a Senate Sponsor of separate bills. Together they formulated what eventually became known as the Comprehensive Addiction and Recovery Act (CARA Act). John along with various VSOs, then assisted to pass earlier versions and then the completed Comprehensive Addiction and Recovery Act. Among other activities, this legislation is the ordered initiation of pilot programs on complementary medicine modalities.
John also worked with US Congress to initiate a Government Accountability Office Investigation (GAO) that resulted in the GAO findings, that there was no VA evidence that veterans were informed of both the side effects of medications and the treatment options that were available.
He also initiated legislation to analyze if there were links between veteran suicides and medications that carried a black box warning.
Part of his legislation was tagged onto the National Defense Authorization Act. It was then passed by both Houses of Congress and signed into law by the President. It caused the National Academy of Science, Engineering, and Medicine to carry out a study, into veteran suicides and whether there exist any links to opioids and benzodiazepines.
It is essential that medical doctors reinstate their optimum operating basis:
First, do no harm. Perform a comprehensive case history. And then follow this up with a differential diagnosis (eliminate all possible causes, until the correct cause is isolated and confirmed).
John views a correct diagnosis as foundational. This is key to resolving the underlying problem and as a result, the veteran’s symptoms.
It is the treatment of symptoms, with medications, that can create more symptoms, that should be scrutinized. The medications may provide needed temporary relief. However, it is still crucial to tenaciously pursue the source of the ailment. Such is in the best interest of the veteran. Doing so also will result in a true appreciation and confidence in the medical establishments and medical system in general.
——————————————————————————————————————
Veterans Service Organizations join with Veteran Strategic Solutions in supporting Written Informed Consent:
Written Informed Consent – An Introduction
Many of these drugs are prescribed for our most fragile veterans and they often carry suicidal ideation as one of their main side effects. Making matters worse, many of these same veterans are often prescribed more than one of these risky medications. We support using these medications if they are medically necessary, the benefits outweigh the risks, and the physician clearly explains the potential risks/alternate treatment options so that the veteran understands what to expect while taking the medication(s).
Problem: Imagine a fragile veteran, taking one or more of these powerful and risky medications, who is not prepared for possible side effects such as: vision problems (blurred or unfocused); hallucinations (seeing things or hearing voices); depression; anger issues; severe fatigue; being unable to think/function coherently, etc. Any or all of these could push them over the edge into a possible suicidal situation due to fear or confusion. Furthermore, they may be unable to work or support themselves and their families, they may be dealing with alcohol or drug addiction, or they might exhibit violent or unpredictable behavior.
Focus: Saving lives by reducing/eliminating veteran (and potentially military) suicide using Written Informed Consent only for Black Box medications included in the VA formulary. Black Box medications are required by the U.S. Food and Drug Administration to carry special warnings for medications that have a high potential for serious safety risks. Often these warnings communicate potentially rare but dangerous side effects, or they may be used to indicate important instructions for the safe use of the drug.
Over the years, the VA (along with the DoD) has spent millions of dollars on veteran and branch-specific suicide prevention programs with little to no success in improving veteran (military) suicide statistics.
Clearly, something is not working as planned. Continuing to do the same failed actions/programs and wasting finite financial resources is the definition of insanity. It is time to try something simple, different, and cost-effective.
As a first step we need to enforce what is already a part of the VHA Handbook: “Veterans must be informed of the side effects and the treatment options of medications and treatments they are prescribed.”
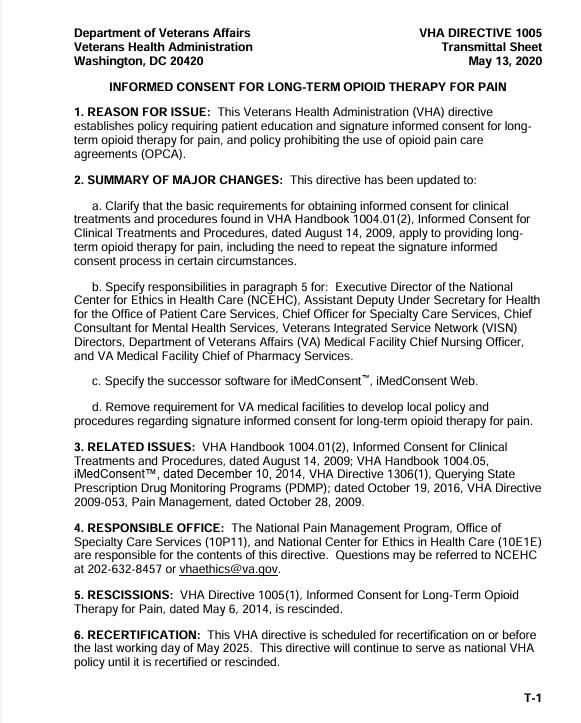
Unfortunately, according to the VHA Handbook, Verbal Informed Consent is the standard for medications for veterans (see also – VHA Directive 1005: Informed Consent for Long-term Opioid Therapy for Pain). What is the problem with verbal only consent? There’s no way to track that sufficient and understandable information regarding medication is being provided to veterans. In fact, there’s no way to verify that the veteran is getting more information than what is provided, in unintelligible language, in the medication insert. Even VA pharmacists do not consistently provide in-depth information regarding side effects, etc.
Because Verbal Informed Consent cannot be monitored, it is not enforceable. This oversight causes our veterans and their families to be subject to a lack of vital information about medication side effects as well as their right to be aware of, and possibly choose other medications or treatment options.
Additionally, the veteran’s inability or desire to work, familial and spousal disputes, unanticipated health problems, and homelessness may also stem from the side effects of these Black Box medications and/or polypharmacy.
Solution: Written Informed Consent will help ensure that clinicians are providing all vital information, including risks and side effects, considering all available evidence-based treatment options and medications to each veteran as a means of minimizing or eliminating the potential risk of suicide. This extra step should not only increase adherence to the treatment regimen but will prepare veterans for what they may expect during their treatment thereby removing the fear factor that could push them toward suicide. The combination of patient education and Written Informed Consent prior to prescribing helps to ensure that patients and their providers have a shared understanding of the patient’s goals and the risks, benefits, and alternatives.
——————————————————————————————————————
2023 JWV Resolutions
1WRITTEN INFORMED CONSENT RESOLUTION
2WHEREAS, A Bill to amend title 38, United States Code, to direct the Secretary of Veterans
3Affairs to establish and maintain a current and up-to-date database of all drugs within the VA
4formulary that carries an FDA Black Box warning and to all VA medical facilities to require
5signatory informed consent when prescribing any of those medications is being introduced in the
6House of Representatives of the United States; and
7WHEREAS, The 2021 Veterans Health Administration (VHA) Handbook Directive 1004.01(5)
8states that it is sufficient to obtain oral consent for the entire treatment or procedure without
9explicitly discussing each of its component elements for procedures that are low risk and within
10universally accepted standards of medical practice; and
11WHEREAS, Starting back in 1976, the Food and Drug Administration (FDA) started
12generating a prominently labelled black box warning (BBW) label to warn of serious life-
13threatening risks associated with market-approved prescription drugs or medical devices; and
14WHEREAS, VA Office of Inspector General (OIG) noted back in 2019 an increased risk of
15adverse outcomes such as drug interactions and overdose, as well as diversion of opioids
16to nonpatients, due to the lack of conducting state’s prescription drug monitoring program
17(PDMP) queries and inconsistent electronic health record documentation; and
18WHEREAS, The Government Accountability Office (GAO) found in 2019 that the Department
19of Veterans Affairs (VA) failed to monitor whether VA mental health providers in
20specialty care documented the required consideration of different treatment options, such as
21psychotropic medications or non-pharmacologic therapy, within mental health treatment plans;
22and
23WHEREAS, A GAO 2018 report already recommended for the VA to obtain written informed
24consent on use of opioids, so that veterans may have an informed understanding of the risks and
25benefits, as already required by VHA policy; and
1WHEREAS, A high percentage of the veteran population suffer from post-traumatic stress
2disorder, anxiety and/or depression; and
3WHEREAS, By 2017, certain VA Veterans Integrated Services Networks (VISN) already
4erected a dashboard for opioid monitoring; and
5WHEREAS, Certain antidepressants such as Bupropion (marketed as Wellbutrin), have gained
6scrutiny for not only an increased risk for suicide ideation, but also for carrying a warning label
7for symptoms including “abdominal pain, constipation, decrease in appetite, dizziness, dry
8mouth, increased sweating, nausea or vomiting, trembling or shaking, trouble sleeping,
9weight loss, blurred vision, change in sense of taste, drowsiness, the feeling of fast or
10irregular heartbeat, frequent need to urinate, unusual feeling of well-being, agitation, anxiety,
11tinnitus, skin rash, hives, itching, confusion, extreme distrust, hallucinations, seizure, and trouble
12concentrating”; and
13WHEREAS, Current VHA Handbook directives do not currently ensure consultations of high-
14risk medications, especially those carrying an FDA BBW, are consistently carried out and
15documented in a veteran’s electronic health record.
16THEREFORE, The Jewish War Veterans of the USA supports and requests immediate passage
17by the Congress of the United States the Bill to amend title 38, United States Code, to direct the
18Secretary of Veterans Affairs to establish and maintain a current and up-to-date database of all
19drugs within the VA formulary that carries an FDA Black Box warning and to all VA medical
20facilities to require signatory informed consent when prescribing any of those medications is
21being introduced in the House of Representatives of the United States; and,
22FURTHERMORE, That the Department of Veterans Affairs (VA) to create a national standard
23of practice for all Veterans Integrated Services Networks regarding black box warning (BBW)
24monitoring; and,
25FURTHERMORE, That VA routinely ensure that VA providers are conducting state prescription
1drug monitoring program queries to avoid adverse health outcomes and
2that the VA implement a signatory documentation policy between prescribing provider and the
3patient or caregiver when prescribing BBW medications to ensure they are properly informed,
4and the severity of potential risks are adequately presented; and,
5FURTHERMORE, That any negative health outcomes or risks associated with the use of BBW
6medications are properly tracked for further study and recorded in a manner that is publicly
7available and easily accessible; and,
8FURTHERMORE, That VA implement a mandatory and prompt follow-up wellness check
9schedule for veterans receiving BBW medications.
——————————————————————————————————————
NATIONAL EXECUTIVE COMMITTEE OF THE AMERICAN LEGION
May 10-11, 2023 Indianapolis, Indiana Resolution No. 18:
Written Informed Consent
Origin: Veterans Affairs & Rehabilitation Commission Submitted by: Veterans Affairs & Rehabilitation Commission
WHEREAS, Latest 2021 Veterans Health Administration (VHA) Handbook Directive 1004.01(5) states that it is sufficient to obtain oral consent for the entire treatment or procedure without explicitly discussing each of its component elements for procedures that are low risk and within broadly accepted standards of medical practice; and
WHEREAS, Starting back in 1976, the Food and Drug Administration (FDA) started generating a prominently labelled black box warning (BBW) label to warn of serious life-threatening risks associated with market-approved prescription drugs or medical devices; and
WHEREAS, VA Office of Inspector General (OIG) noted back in 2019 an increased risk of adverse outcomes such as drug interactions and overdose, as well as diversion of opioids to nonpatients, due to the lack of conducting state’s prescription drug monitoring program (PDMP) queries and inconsistent electronic health record documentation; and WHEREAS, The Government Accountability Office (GAO) found in 2019 that the Department of Veterans Affairs (VA) failed to monitor whether VA mental health providers in specialty care documented the required consideration of different treatment options, such as psychotropic medications or non-pharmacologic therapy, within mental health treatment plans; and
WHEREAS, A GAO 2018 report already recommended for the VA to obtain written informed consent on use of opioids, so that veterans may have an informed understanding of the risks and benefits, as already required by VHA policy; and
WHEREAS, A high percentage of the veteran population suffer from post-traumatic stress disorder, anxiety and/or depression; and
WHEREAS, By 2017, certain VA Veterans Integrated Services Networks (VISN) already erected a dashboard for opioid monitoring; and WHEREAS, Certain antidepressants such as Bupropion (marketed as Wellbutrin), have gained scrutiny for not only an increased risk for suicide ideation, but also for carrying a warning label for symptoms including “abdominal pain, constipation, decrease in appetite, dizziness, dry mouth, increased sweating, nausea or vomiting, trembling or shaking, trouble sleeping, weight loss, blurred vision, change in sense of taste, drowsiness, the feeling of fast or irregular heartbeat, frequent need to urinate, unusual feeling of well-being, agitation, anxiety, tinnitus, skin rash, hives, itching, confusion, extreme distrust, hallucinations, seizure, and trouble concentrating”; and
WHEREAS, Current VHA Handbook directives do no currently ensure consultations of high risk medications, especially those carrying an FDA BBW, are consistently carried out and documented in a veteran’s electronic health record; now, therefore, be it RESOLVED, By the National Executive Committee of The American Legion in regular meeting assembled in Indianapolis, Indiana, on May 10-11, 2023, That The American Legion urges the Department of Veterans Affairs (VA) to create a national standard of practice for all Veterans Integrated Services Networks regarding black box warning (BBW) monitoring; and, be it further RESOLVED, That VA routinely ensure that VA providers are conducting state prescription drug monitoring program queries to avoid adverse health outcomes; and, be it further RESOLVED, That VA implement a signatory documentation policy between prescribing provider and the patient or caregiver when prescribing BBW medications to ensure they are properly informed, and the severity of potential risks are adequately presented; and, be it further
RESOVLED, That any negative health outcomes or risks associated with the use of BBW medications are properly tracked for further study and recorded in a manner that is publicly available and easily accessible and, be it finally RESOLVED, That VA implement a mandatory and prompt follow-up wellness check schedule for veterans receiving BBW medications.
——————————————————————————————————————
——————————————————————————————————————

Honorable Congressman Cory Mills (Fl-07)
!237 Longworth House Office Building
Washington, D.C. 20003
Dear Honorable Congressman Mills, March 4, 2024
Our Legislative Committee Chairman of the Association of the United States Navy, LCDR Dave Bradley has reviewed your bill, Veterans Informed Consent Act, and is pleased to inform you that on behalf of our organization he fully supports it.
Today, we are living in extraordinary times that are bringing to our veteran’s extraordinary challenges like no other time in recent history.
Unfortunately, the suicide rate is climbing, depression and mental disorders among the ranks of all military services is increasing, and treatment and care is not at its best.
It was President George Washington who said, “A nation is indeed judged by how it treats its veterans.” And someone else once said, “The way we honor and support those who have served in our armed forces reflects our collective character and values.”
Sometime ago, I read in an article about health care for veterans this statement, “The willingness of our young people to serve in times of war is directly linked to their perception of how veterans from earlier conflicts were treated and appreciated by our nation. When veterans receive the respect, care, and recognition they deserve, it inspires future generations to step forward and defend their country. Conversely, when veterans face challenges, neglect, or hardship, it can dampen the spirit of service.”
Your Bill, Veterans Informed Consent Act is a giant step in the right direction. A well-informed patient about the care, treatment, and medication they are prescribed will minimize if not eliminate side effects that will cause greater harm to them.
Your Bill is a WIN, WIN for everyone concerned.
Kind regards,
Steven Rogers
LCDR Steven Rogers, US (Ret)
AUSN
——————————————————————————————————————
August 4, 2023
John Spagnola, President/CEO
Veterans Strategic Solutions
675 S. Gulfview Blvd., Ste. 204
Clearwater, FL 33767
Dear John,
Thank you for contacting Vietnam Veterans of America requesting our opinion on the proposed legislation: To amend title 38, United States Code, to direct the Secretary of Veterans Affairs to establish and maintain a current and up-to-date database of all drugs within the VA formulary that carry a Food & Drug Administration (FDA) Black Box warning and shall further require all VA medical facilities to require signatory informed consent when prescribing any of those medications.
The current law is clear about VHA’s requirement for full and informed consent. 39 USC Chapter 73: Veterans Health Administration-Organization and Functions, Subchapter III – Protection of Patient Rights, §7331 Informed consent.
The Secretary, upon the recommendation of the Under Secretary for Health and pursuant to the provisions of section 7334 of this title, shall prescribe regulations establishing procedures to ensure that all medical and prosthetic research carried out and, to the maximum extent practicable, all patient care furnished under this title shall be carried out only with the full and informed consent of the patient or subject or, in appropriate cases, a representative thereof.
However, what are VHA’s policies and procedures regarding the requirement for full and informed consent? How are they systematically deployed, and how consistent are they? Furthermore, what are their specific policies and procedures regarding consent for safe medication administration?
When enacted, the proposed bill would give the VA Secretary 180 days to see that all VA medical facilities are tracking the proper usage of the signatory informed consent requirement to evaluate the outcomes. Within 270 days of enactment, VA would be required to report their findings to the House & Senate Veterans Affairs committees. The bill also pushes information and counseling on veterans but does not allow them to opt out. VVA suggests that the bill include language to that effect.
VVA supports the proposed legislation to be introduced in the 118th Congress, stipulating signatory informed consent with relevant information and counseling available to the veteran, thus ensuring VA follows guidelines to minimize the risk to veterans when they are prescribed any black box medications.
Sincerely,
Jack McManus